Breast cancer is the most common cancer among women in Singapore, with one in 13 women expected to be diagnosed in their lifetime. As general practitioners (GPs) play a vital role in early detection, it is crucial to understand the national screening guidelines and the rationale behind them.
Our consultant radiologist, Dr Eugene Ong, provides an overview of breast cancer screening recommendations, including why screening starts at 40, the role of ultrasound, the differing screening intervals for various age groups, and key imaging concepts such as BI-RADS and indeterminate lesions.
Screening and Diagnosis
Early Detection through regular screening can significantly increase the chances of successful treatment and survival. By detecting breast cancer at an early stage, treatment options are usually less invasive, and the prognosis is generally more favourable.
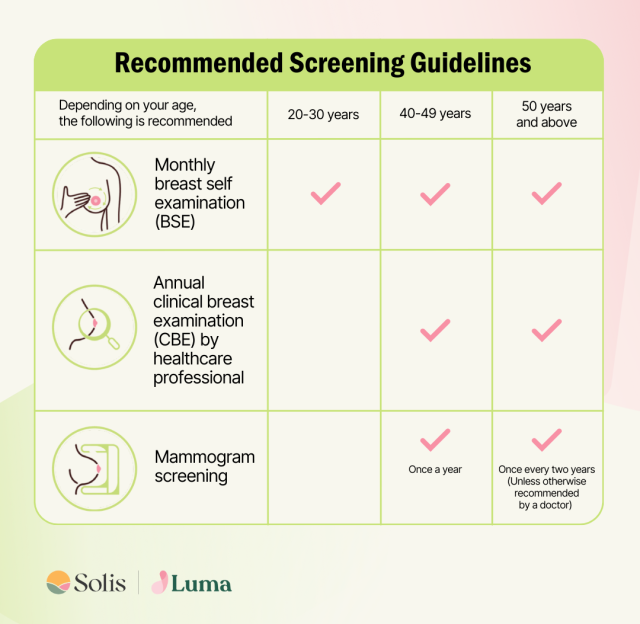
Note: Age recommendations are only guidelines and may differ for those with a family history of breast cancer or those who have other risk factors. Supplementary ultrasound may be ordered to increase the accuracy of screening.
1. Why Screen at 40 Years Old vs. 50 Years Old?
- Early Detection: Screening from age 40 allows earlier detection of breast cancer, which is crucial as breast cancer can develop before 50. Studies have shown that Asian women, including Singaporean women, tend to develop breast cancer at a younger age compared to Western populations.
- Higher Incidence in Younger Women: In Singapore, a not-insignificant proportion of breast cancer cases occur in women in their 40s. Screening from 40 helps detect cancers earlier when they are more treatable.
- Survival Benefit: Early detection through screening in women aged 40–49 has been associated with improved survival rates and reduced mortality.
- Government Guidelines: The Ministry of Health (MOH) and the Singapore Cancer Society recommend mammogram screening starting at 40, with different screening intervals depending on age (see point 3).
2. Why Screen with Ultrasound – Why Isn’t Ultrasound in the MOH Guidelines, Only Mammograms?
- Mammograms are the Gold Standard: Mammography is the only breast screening method with proven mortality reduction in large-scale population screening. It effectively detects microcalcifications, which can be an early sign of breast cancer.
- Ultrasound as a Supplemental Tool: Ultrasound is useful in women with dense breasts (common in younger women and Asian populations) as mammograms may miss some cancers in dense breast tissue. However, ultrasound alone is not a primary screening tool because it is operator-dependent and can lead to higher false positives.
- MOH Guidelines Prioritize Evidence-Based Screening: Since large-scale randomized trials have not proven ultrasound as an effective stand-alone screening tool, it is not included in national guidelines. However, in clinical practice, ultrasound is often recommended as an adjunct to mammography, especially for women with dense breasts.
3. Why Do We Do Increasing Intervals for Mammogram Screening (Annually for 40-49 Years, Every 2 Years for 50+)?
- Changes in Breast Tissue Composition: Glandular tissue appears white on mammograms, while fatty tissue appears black. As women age, glandular tissue involutes and is replaced by fatty tissue.
- Challenges in Detecting Cancer in Younger Women: Since breast cancers also appear white on mammograms, they can be more easily obscured by dense glandular tissue in younger women. More frequent mammograms (annually from 40-49 years) help improve detection.
- Improved Visibility in Older Women: As women age, their breasts contain more fatty tissue, providing better contrast for detecting white cancerous lesions against the black fatty tissue background. Hence, mammograms can be performed less frequently (every two years from 50 onwards).
4. What is an Indeterminate Lesion?
- Definition: An indeterminate lesion is a breast abnormality detected on imaging that cannot be definitively classified as benign or malignant. It requires further evaluation, which may include additional imaging (e.g., ultrasound, MRI) or biopsy.
- Examples: Small solid masses, complex cysts, or lesions with ambiguous features on mammography or ultrasound.
- Follow-up: Some indeterminate lesions will require further evaluation by breast specialists, while others may need biopsy to confirm the diagnosis.
5. What is BI-RADS?
When you undergo a mammogram, ultrasound or MRI, our radiologists categorise the findings to communicate the recommended follow up actions.
Your report will likely include a BI-RADS score, which is a standardised system used to classify findings and guide recommendations. BI-RADS (Breast Imaging- Reporting and Data System) is a standardised system developed by the American College of Radiology (ACR) to categorise breast imaging findings and their level of suspicion for malignancy ranging from 0 to 6.
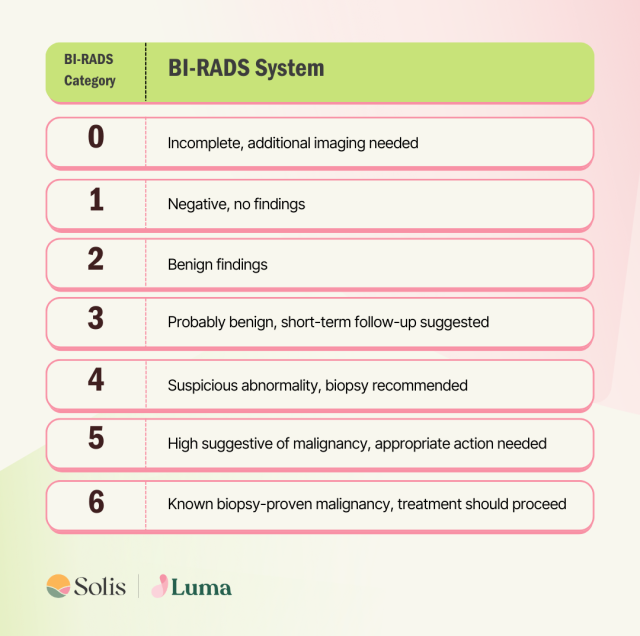
At times, it may be difficult to classify findings into BI-RADS 0-6, so some centres use descriptive terms instead- such as benign, probably benign, indeterminate, or suspicious. This helps guide the breast surgeon on the next steps. [Ref: American College of Radiology]
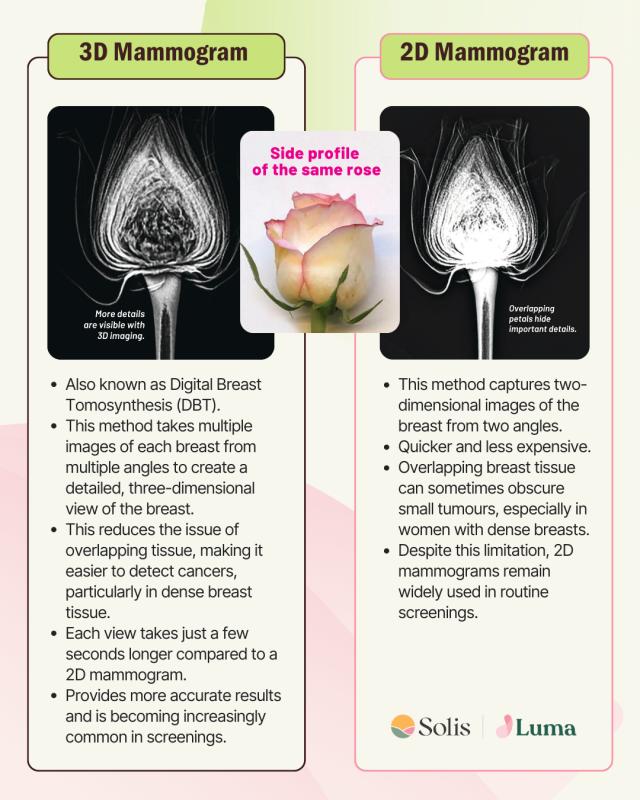
3D Mammogram vs 2D Mammogram
Mammograms are X-ray images of the breast used to detect tumours or abnormalities, and are the most common screening tool for breast cancer. During a mammogram, your breasts are compressed between two plates to capture clear images. While this may be uncomfortable, mammograms are quick and generally painless.
This article has been reviewed by Dr Eugene Ong, Consultant Radiologist at Luma Women’s Imaging Centre




